Maternal Health Awareness Day: Why the U.S. Must Do Better—Especially for Black Mothers
Maternal Health Awareness Day: Why the U.S. Must Do Better—Especially for Black Mothers
Maternal Health Awareness Day forces us to confront the systemic failures that continue to endanger people during pregnancy, childbirth, and the postpartum period. Even as medical innovation advances, maternal outcomes in the United States remain deeply unequal, with Black women facing the most severe consequences.
The state of maternal health reveals a deeper truth about our systems: whose lives are protected by them and whose suffering is treated as acceptable collateral.
The U.S. Has the Worst Maternal Mortality Rate Among High-Income Countries
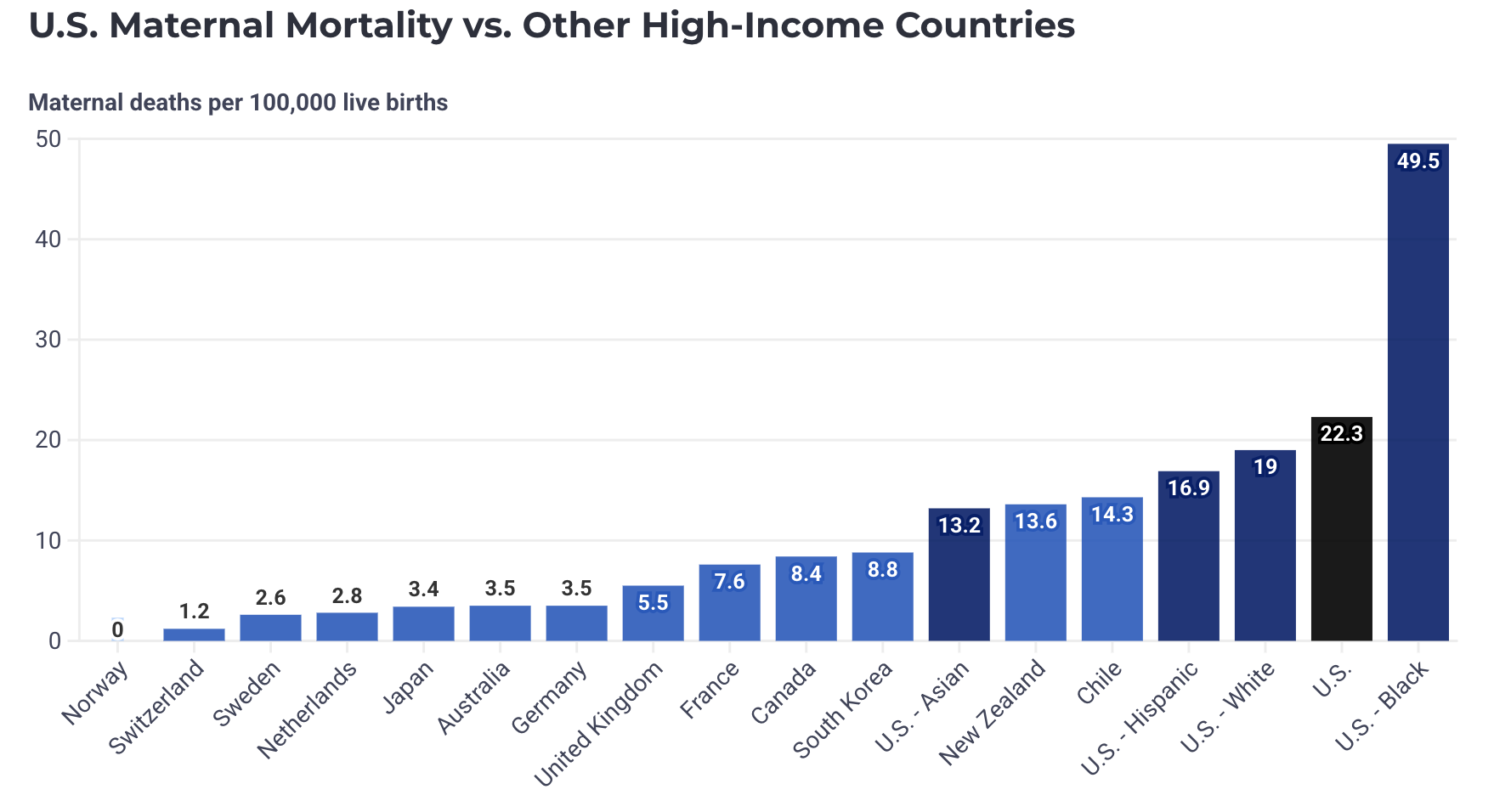
The United States has a maternal mortality rate of 22.3 deaths per 100,000 births, the highest among all high-income countries.
To put that into perspective:
Norway reported zero maternal deaths in 2022
Switzerland reported 1.2 deaths per 100,000 births
In more than half of high-income countries, maternal mortality rates are below 5 per 100,000
The U.S. rate is double—and sometimes triple—that of similar high-income countries. Compared to countries like Sweden, Japan, the United Kingdom, and the Netherlands, maternal deaths in the U.S. occur at three times the rate.
This isn’t a question of medical advancement or resources. It’s a question of systems, priorities, and accountability.
Racial Disparities in Maternal Health
Racial disparities in maternal health are not accidental. They are structural, entrenched, and lethal.
In the United States, Black women die from pregnancy-related causes at a rate of 49.5 per 100,000 births—nearly three times that of white women. These outcomes persist regardless of income, education, or professional status, underscoring that socioeconomic “protection” does not shield Black women from harm.
There is no benign explanation for this reality. What the data reflects is a system that routinely discounts Black women’s pain, delays care, and normalizes preventable risk. Black mothers are not dying because pregnancy is inherently dangerous; they are dying because the systems meant to keep them safe are not built to do so.
Dr. Janell Green Smith
We recently lost Dr. Janell Green Smith—a Black midwife, physician, and women’s health advocate—who died at 31 after giving birth to her first child. She dedicated her life to helping Black women give birth safely, with dignity and trust. And despite her knowledge, training, and advocacy, our healthcare system failed her.
Dr. Green Smith entered midwifery out of righteous frustration with the state of Black maternal mortality. She once shared that she wanted to be “part of the solution—to step into a role as the provider who would listen when patients said they were in pain.” She became that provider for countless families.
Her death is not just a personal tragedy—it is a devastating indictment of a system that continues to put Black women at risk, regardless of education, profession, or proximity to care. Her story makes one truth painfully clear: in this country, systemic racism in healthcare is deadly—even for those who have dedicated their lives to changing it.
Systemic Causes Behind Racial Disparities
The disproportionately high maternal mortality rate among Black women has nothing to do with biology. It is a direct reflection of the systems that too often fail to listen and protect.
Systemic Racism & Implicit Biases: Long-standing medical myths and racial bias, including false beliefs about pain tolerance, continue to shape clinical decision-making today. Black women are less likely to have their symptoms taken seriously, more likely to have pain minimized or dismissed, and more likely to experience dangerous delays in treatment.
Inequitable Access to Quality Maternal Care: Access to consistent, high-quality maternal care is shaped by geography, income, and policy. Many Black women live in maternal care deserts, face transportation barriers, or lack nearby obstetric providers—making timely prenatal and delivery care harder to access.
Fragmented Healthcare System & Insurance Gaps: Unlike other high-income countries with far lower maternal mortality rates, the U.S. does not have a universal healthcare system, leaving coverage tied to employment, income, or pregnancy status. Black women are more likely to experience gaps in insurance before, during, and especially after pregnancy, disrupting continuity of care and delaying critical follow-up services.
Postpartum Care Gaps: Roughly two-thirds of pregnancy-related deaths occur after childbirth, yet postpartum care in the U.S. is often limited, fragmented, or inaccessible. These gaps disproportionately impact Black mothers, especially those on Medicaid, often leaving critical health needs unmet during the most vulnerable period.
Prevention is Possible
More than 80% of pregnancy-related deaths in the United States are considered preventable. This means lives are being lost not because complications are unavoidable—but because warning signs are missed, care is delayed, and follow-up falls through.
Much of prevention begins with empathy—truly listening to patients, validating their pain, and actively addressing implicit bias within healthcare systems. When we look to other high-income countries with far lower maternal mortality rates, the path forward is clear: continuity of care, extended postpartum coverage, and guaranteed paid parental leave aren’t luxuries, they’re essential to protecting the health and lives of mothers in this country.
We know what works. We must continue the fight for equitable healthcare, especially for Black mothers.
What Must Change
Improving maternal health outcomes—especially for Black mothers—requires more than awareness. It demands structural change.
That means expanding postpartum coverage, investing in community-based and midwifery care, addressing maternal care deserts, and confronting bias within medical education and practice. And it certainly means trusting patients when they speak about their own bodies.
The United States has the knowledge, resources, and responsibility to protect mothers. What we lack is the collective will to dismantle the systems that allow preventable deaths to continue.
At Comma, we know that data and education are powerful—but they must be met with systems that listen and care. On Maternal Health Awareness Day, we honor the mothers we’ve lost, including Dr. Janell Green Smith, and recommit to building a future where pregnancy and childbirth are not life-threatening—especially for Black women. Awareness is the first step. Accountability must follow.
Sources:
The Commonwealth Fund: Maternal Mortality in the United States, 2025
World Health Organization: Maternal Health
Central Intelligence Agency: Maternal mortality ratio
U.S. News and World Report: Maternal Mortality: How the U.S. Compares to Other Rich Countries
The Commonwealth Fund: Insights into the U.S. Maternal Mortality Crisis: An International Comparison
CNN: A midwife’s death days after childbirth complications reignites the conversation around Black maternal health
KFF: Five Facts About Black Women’s Experiences in Health Care